
Connecting COVID patients to their families with the support of the community
During the peak of the COVID-19 pandemic, Maureen Hayes, an ICU registered nurse at South Shore University Hospital (SSUH), proposed a brilliant idea of knitting pairs of hearts for COVID patients and their families. One of the hearts would be given to a patient and the other to a family member, allowing them to feel connected although they are apart. She brought the idea to nursing leadership who thought her idea embodied Northwell’s value of being Truly Compassionate and was excited to see it come to life. This was the beginning of the Connected Hearts Project.
The support of our community and teamwork
Both Maureen and her assistant manager, Andrea Freudenberg, were excited about the Connected Hearts Project but needed help getting started. That’s when Andrea reached out to the community for help in creating as many “connected hearts” as possible. Andrea was already a member of the Facebook group ‘The Islip’s Feed Southside Hospital Employees’ and during the height of COVID, their members donated money and ordered from local restaurants to help feed the staff at South Shore University Hospital, formally known as Southside Hospital. She knew this group would be more than willing to lend a hand with this effort.
The response was overwhelming. The outpouring of love and a united community was incredible. Once the hearts began to pour in, the team members in the ICU were able to distribute them.
“Since its launch in April 2020, our Connected Hearts Project has taken on a life of its own,” says Andrea. The Connected Hearts Group at SSUH has monthly meetings with ICU nurses who continue to come up with ideas to support and comfort their patients. This group not only distributes hearts to COVID patients and families but also to other families who are unable to see their loved ones.
The Connected Hearts Project is still new, but it has created a positive impact on our community, patients, families, and our team members. Members of the Facebook group have commented: “It helped me to feel useful during tough times” and “I was happy to be a part of this project.” SSUH team members have also commented that they love having the ability to provide family with a connection to their loved ones.
At Northwell Health, we’re dedicated to supporting team members’ interests above and beyond their day-to-day responsibilities. It allows team members to be creative while delivering compassionate care to their patients and partnering with the community.
Raise Health in our communities where we live, love and work. Apply today!
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Healthcare workers reflect on one year of delivering care throughout the COVID-19 pandemic
March marked one year of our Northwell Health team members delivering care throughout the COVID-19 pandemic, a disease that has impacted our world on an unprecedented level. While the past year has been like no other, our team members have come together to become health raisers. Throughout it all, they have been a bright light of hope amidst some of the darkest times. We asked our team members to take a moment to reflect on their thoughts and feelings on what the past year has meant for them and how they’ve grown.
Read the reflections of our healthcare heroes:
“I am forever changed as a healthcare professional. It was difficult watching all of our patients come into the hospital alone without the support of their families. It has changed me as a nurse to also be their support system and make being in the hospital less scary for them.”
“I have learned that I need to take time for self-care in order to be a better me, including a better ‘work me’. I’m really happy our workplace supports that.”
“I learned that we are able to fight anything. Northwell has made us all strong in fighting this pandemic. We learned to take care of ourselves along with our patients and we will continue to Raise Health.”
“Throughout the past year, we’ve been inspired by our patients. Their recovery is our recovery. Their hope is our hope. In those dark times they were beams of light. Together we will persevere.”
“I have learned to really appreciate the impact we make for our patients, even working remote or in an office. COVID reminded us of the role each and every one of us has in helping patients get better.”
“This past year has shown me how awesome my Northwell coworkers are. When faced with challenges, we rise to the occasion. I am still in awe of the dedication and compassion they have not only shown the patients but each other as well. I hope to never face a healthcare challenge like this again, but I take comfort in knowing that my Northwell family will be there to get us through it!”
“My whole life has changed tremendously since last March. Since being redeployed from my role as a standardized patient, I have worked with Workforce Safety on mask fit testing, met the nurses and support staff at different hospitals, mobile units and vaccine pods, and came to know church leaders in faith-based testing. With the unflagging, determined and courageous support of our outstanding Community Relations team, I and many others like me have had our eyes opened to the tremendous amount of goodwill, generosity of spirit, and all-encompassing empathy that our Northwell family possesses – and we are all so much the better for it.”
“Scientists and researchers are ‘behind the scenes’ healthcare heroes and this year I felt even more proud of being a medical researcher. It was empowering to see how the complex biology questions scientists spent time understanding and the knowledge/techniques they discovered eventually came together to produce and distribute the vaccines that are giving us hope that we can end this.”
“Being a respiratory therapist over this past year, in the height of a pandemic, has taught us to be creative in problem solving, to provide the bestcare for our patients during uncertain times and promote a positive working environment during the darkest hours. It has taught me the ability to positively influence coworkers and teammates to work together for a common cause and mission.”
“As an MRI radiology manager, my job changed dramatically (during COVID) as we focused on keeping patients safe during MRIs. COVID has given me a greater sense of pride than anything else I dealt with in over 20 years of my career. As a leader I watched my team step up in ways that I couldn’t imagine.”
“These unprecedented times have changed me as a healthcare hero in that I have gained a tremendous amount of respect for every single role within the system. I have witnessed heroism from everyone and I feel lucky to play a small role in a community that exudes cohesiveness, unity and respect – which was so palpable throughout the past year.”
Join our team members as they Raise Health in the communities where we live, love and work. Apply today!
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Northwell Health remembers and spreads the light of our fallen heroes due to the COVID-19 pandemic
This March marked one year since Northwell treated the first case of COVID-19. While it has been a challenging year for all of us, the perseverance of our frontline heroes, the power of science, and the hope of ongoing vaccinations and innovative treatment plans brings us comfort for the path ahead.
The most difficult challenge has been coping with the grief associated with the loss of our colleagues, friends, family members and those in our communities. From March 9 to March 14, Northwell held remembrance activities to “spread the light” for our fallen team members and those who we have lost due to COVID-19. New York City – the epicenter of this pandemic – has also declared Sunday, March 14, as a Day of Remembrance to honor everyone we’ve lost.
To spread the light throughout our remembrance week, team members were encouraged to wear blue in memory of those who worked at Northwell and as a show of solidarity for our Northwell community. On site, our chaplains hosted moments of silence and remembrance circles to help our team members find meaning, hope, connection and comfort through togetherness regardless of religious affiliation. Spread the light activities were also available at our facilities, allowing team members to reflect by writing messages on remembrance boards, prayer cards, and lighting luminary bags to symbolize fallen team members.
Team members and their families also continued to spread the light in our communities over the past week as they organized light parades in their neighborhoods, created luminary bags and took a moment to pause to reflect with their loved ones.
During our remembrance week, Northwell also held an organization-wide Town Hall featuring our President and CEO, Michael Dowling, and other senior leaders, to connect our 75,000 team members and speak about the strength and sacrifice of our healthcare heroes. In addition to honoring those we have lost, it also recognized the efforts and unwavering dedication of our team members throughout the pandemic. From March 12 to March 14, our corporate headquarters in New Hyde Park, New York was illuminated in blue to honor our fallen team members and recognize the enduring courage and spirit of our Northwell community.

Throughout these challenging times, Northwell has also supported our team members by expanding benefits, offering prayer groups and providing well-being resources from our Team Lavender, a program at Northwell that provides staff with an opportunity for timely emotional, spiritual and physical support. These resources, such as Tranquility Tents, which offered areas of respite for our hospital workers during their shifts, and opportunities for 1:1 counseling through our Employee Assistance Program, have allowed for us to care for our team members as they delivered care to our communities. A 24/7, free and confidential, emotional support call center for all team members and their families also provided emotional well-being experts to answer their questions, provide additional resources, or just listen.
At Northwell Health, we will continue to battle this pandemic, look forward to brighter days, and support our team members.
We will always remember our brave fallen team members and their families. Join us as we spread the light.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Northwell nurse newlyweds deliver heartfelt care to our community
When Vanessa Baral, BSN, RN, and Herwyn Silva, BSN, RN, CEN, first met over a decade ago, their shared nursing experience helped them to bond. Today, their love for nursing—now as Northwell employees—continues to complement their love for each other as they begin their married life together.
Though they work in separate Northwell hospitals and units, Vanessa in the ICU at LIJ Forest Hills and Herwyn in the Emergency Department at Lenox Hill Hospital, they appreciate how their shared profession helps them to understand each other on a different level. This unique insight became especially valued as they both cared for COVID-19 patients at their hospitals at the start of the pandemic last March.
“Both of us being RNs is very comforting, especially in these different times. In the ICU and ED, we work with some of the sickest patients and see things most people don’t see or go through,” says Herwyn. “Having that support person at home who knows what you go through at work is very comforting.” Vanessa agrees adding, “We can support each other whenever we have a rough day at work or at home knowing that we have been there and that we are doing it together.”

Hoda Kotb officiates Herwyn and Vanessa’s socially distant wedding live on the Today Show
And while they delivered care to our patients during this unprecedented time, Vanessa and Herwyn also made the difficult decision to put their wedding plans, originally scheduled for May 17, 2020, on hold to ensure the safety of their family and loved ones. Life, however, had other plans in store for them. In a celebration of their work as healthcare heroes on the front-lines, Vanessa and Herwyn were given the once-in-a-lifetime opportunity to have their wedding ceremony live on the Today Show on June 25th, 2020, ordained by Hoda Kotb herself.
After their wedding, they continued to deliver compassionate patient care and today they also serve in another role as nurses: working at our vaccination sites. Distributing vaccines allows them to deliver hope to patients in the form of a brighter tomorrow while working side-by-side.
“Distributing vaccines is an upbeat and happy moment we share with the community and a break from the difficult situations we sometimes deal with in the ICU and ED,” says Herwyn. “We vaccinated people who were looking forward to finally being able to see grandchildren, to essential workers and group home residents. These moments, full with nerves for some, are also filled with moments of hope and happiness.”
“The past year has been rough for everyone but being a duo has made it easier,” says Vanessa. “From working the frontlines as nurses, getting married live on tv during a pandemic, and now vaccinating our communities, we are happy to share our story with people to just spread joy in times when it feels more needed than ever.”
Discover a career well cared for in the community where you live, love and belong. Apply to Northwell Health today!
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

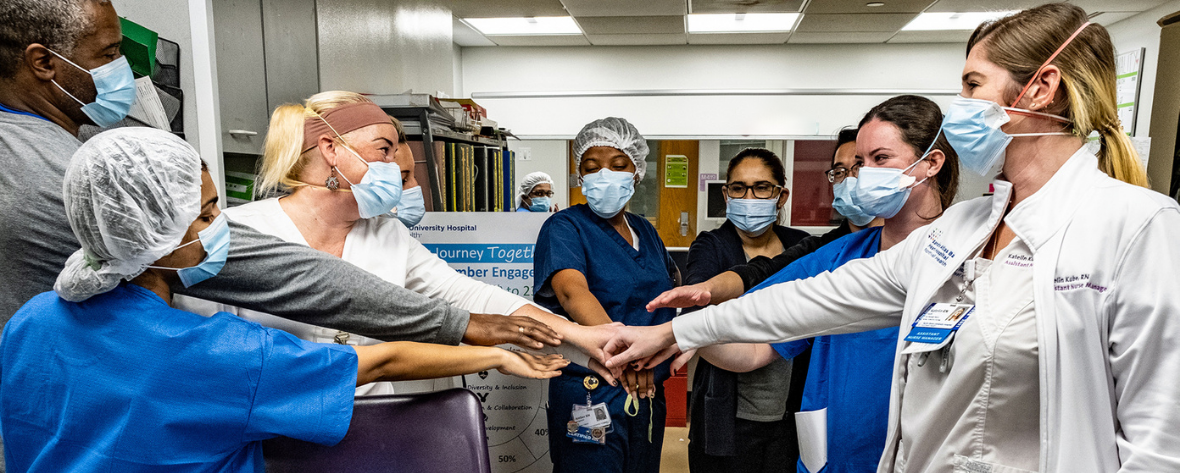
Northwell nurses deliver care at Henry Ford Health System as part of strategic alliance to fight COVID-19
When the COVID-19 pandemic first hit New York, nurses from around the country came to New York to fight on the front-lines alongside our healthcare heroes. Now as the pandemic surges in other states, the nurses at Northwell are returning that same support.
Recently Northwell Health sent 12 intensive care and medical-surgical nurses to Michigan-based Henry Ford Health System to help the clinicians as they cared for a rising number of patients in their system suffering from COVID. This staff-sharing initiative occurred as part of a newly formed strategic alliance between the health systems. In addition to staff-sharing, this alliance allows for collaborative emergency planning and an exchange of best practices, all in an effort to strengthen our ability to fight the new coronavirus and support the health and well-being of our communities.
Northwell’s intensive care and medical-surgical nurses are the first to participate in staff-sharing under this alliance, volunteering for the program to share their knowledge, skills, and provide a boost of morale and support to the nurses currently delivering care during a resurgence of COVID-19.
Fritz-Gerald Lochard, executive program director with the HR Office of the Chief People Officer, first saw the benefits of staff-sharing when he became directly involved with the clinicians who came to support our health system last spring from University of Rochester Medical Center and Intermountain Health in Utah. When he was offered the opportunity to lead the group of nurses on deployment to Michigan, he accepted immediately.
“I felt it was my duty to ensure that our Northwell nurses would have everything they needed while they were leaving their own families behind for a couple of weeks to help save lives,” says Fritz-Gerald. “The entire experience for me personally was a remarkable one for a number of reasons. The individuals at Henry Ford were spectacular and made sure that the nurses and myself had everything we needed to be successful while we were there. The administrative team and staff we all encountered were welcoming and supportive.”
The importance of strategic alliances has only become more apparent throughout the pandemic. As the disease spread, many health systems were severely impacted by staff shortages to support their clinical needs. Staff-sharing not only provides a way to increase staffing in a crisis quickly and efficiently, but provides vital knowledge sharing in an unprecedented time and a boost of morale for both teams.
“Deploying to Henry Ford Health System was extremely rewarding,” says Gina Zinzi, BSN, RN-BC, an ICU nurse at Northern Westchester Hospital. “It felt great to assist a fellow healthcare team who needed an extra set of hands. I would do it again in a heartbeat.”
“I was so excited to be asked to go to Michigan and help out fellow nurses, knowing how much it meant to my ICU when we had nurses from out of state volunteer to come help us,” says Marisa Allen, a registered nurse in Interventional Radiology at Long Island Jewish Medical Center who was asked to deploy due to her ICU background. “The staff at Henry Ford Hospital was so welcoming and it was a great experience getting to work at their facility.”
To Fritz-Gerald, strategic alliances like this only serve as proof that our organization is willing to exhaust all options to ensure those on the front-lines had the support they needed day in and day out. “I think in the environment that we are in now with COVID, it can only assist us in how we deliver care to our respective communities while making our organizations innovative and agile,” says Fritz-Gerald. “I truly learned a lot and I would recommend anyone who has the opportunity to visit another health system to take it!”
Discover a career well cared for at Northwell Health. Apply today!
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

The Integrated Distribution Center makes an impact at Northwell Health during the COVID-19 pandemic
Northwell Health’s Integrated Distribution Center (IDC) located in Bethpage, NY serves a vital role within the organization, especially during the COVID-19 pandemic. The distribution center operates 24 hours a day, 7 days a week, stocks nearly 3,000 unique medical supplies- including personal protective equipment (PPE) and delivers them to 23 Northwell hospitals. It has more than 100 team members who work above and beyond to gather, pack and ship supplies all year round.
Before the pandemic, the center would stock 20 to 30 days’ worth of medical supplies. But with the increase demand of supplies and PPE, the center stocks 90 to 120 days of supplies to prevent any shortages. From the very beginning of the pandemic to now, our hospitals and employees are fully provided with PPE from the distribution center to ensure their safety and that of our patients and community. And now, with the vaccine being administered, the distribution center holds millions of syringes as well.
“Throughout this pandemic, there has been many heartfelt accounts of patients leaving Northwell hospitals with team members cheering and clapping – celebrating Northwell patients’ quick recoveries,” says Paul Spodek, assistant vice president of the Supply Chain Distribution & Logistics Integrated Distribution Center. “When we step back and look at those happy pictures and videos, we notice the isolation gowns, N95s, ear loop masks, etc., all worn by patients and hospital staff alike, every IDC associate knows that all those supplies came from us.”
Each role within the distribution center is unique and valuable to our organization. Our team members all make a difference whether they work the inbound shift where they receive materials and stock shelves to the outbound shifts who picks, packs and load trucks. The IDC also has a support staff who orders and counts supplies and returns, makes sure the distribution center does not run out of materials and manages inventory expiration dates and recalls- they make a difference. “Every IDC team member feels the connection of their role in quality patient care in every Northwell hospital. This connection is the reason why more than 100 team members at IDC have come to work every day during this pandemic and continue to feel great pride in our role in quality patient care,” says Paul. The IDC also creating a better environment for our community. They remove most cardboard and send it to recycle before shipping to our hospitals. The distribution center is on target to recycle more than 220 tons of cardboard in 2020.
The impact and work that our center has on our healthcare heroes and patients is incredible. “As a distribution center associate, and being part of the supply chain, it is a privilege to be helping our doctors, nurses, and the rest of our Northwell heroes by supplying them all the PPE and equipment’ they need to help fight this deadly pandemic,” says Ildebrano Molina.
The teamwork, hard work and dedication of the distribution center showcases the importance of Northwell values. “My entire career has revolved around logistics and distribution but what makes working for Northwell Health`s Distribution Center different is the sense of teamwork and knowing that I am doing something positive for the community that I live in,” says Daniel Pauly, operations manager at the Integrated Distribution Center. “Especially throughout the pandemic, I felt a strong sense of pride and satisfaction knowing that my contribution aided thousands of individuals.”
We are proud of the work that the distribution center has done and continuing to do for our organization and patients.
Discover a career well cared for at Northwell Health. Apply today!
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

A unique start to Emergency Nursing at Northwell Health
Meet Patrick Barnes, a registered nurse in the Emergency Department (ED) Nurse Fellowship at North Shore University Hospital (NSUH). Beginning his nursing career in October just before the COVID-19 pandemic, the initial months of his fellowship provided Patrick with the essential emergency nursing skills to work in a high-acuity, fast-paced emergency department- a unique start to his career.
The ED Nurse Fellowship helps new graduate and registered nurses who may be entering a new specialty gain invaluable skills before working on their own in the ED. As a fellow, Patrick spent the first 10-weeks of his career at Northwell’s Institute for Nursing with classroom education and simulation trainings to teach him the basics of working in the ED and prepare him to start working 12-hour shifts in December.
Working as a new nurse during the COVID-19 pandemic
As our emergency rooms saw a temporary increase in patient volume as the pandemic peaked in March, Patrick found strength from the experienced team around him in the ED. “Our preceptors and the other nurses in our unit have helped the nurse fellows and other new hires prepare for increased patient flow during COVID-19,” says Patrick. “Though demands in our ED would change daily, myself and the fellows I started with were able to adapt tremendously thanks to their support. We would have daily briefs and education to reinforce skills that would keep us and our patients safe.”
While his fellowship continues, the format has changed to keep our team members safe while complying with COVID-19 restrictions. Trainings and certifications are now taught through virtual platforms or while practicing social distancing in small classroom settings. Throughout the unprecedented circumstances, Patrick has never felt the guidance from Northwell and his leadership waver.
Building a future in emergency nursing at Northwell
With his fellowship now nearly over, Patrick feels prepared to start the next stages of his RN career at Northwell. “Within my first year as a nurse, Northwell has given me opportunities and training that I feel I may not have been offered elsewhere,” says Patrick. “It feels like a family once you begin to work with the team in the ED.”
Patrick’s passion for emergency nursing is the foundation for growing his career at Northwell. Working in the ED, he’s seen firsthand how our nurses have moved onto educator and management roles within the system. “It is exciting to see many of our team members move on to earn their MSN and have the support of the ED behind them,” says Patrick. “I am excited to see what the future holds at Northwell.”
Start your nursing career with Northwell Health. Learn more about our nurse fellowship programs.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Rebecca’s experience during COVID-19 in Northwell’s Reassignment Reserve
As COVID-19 peaked throughout New York, Northwell Health took the initiative to create a Reassignment Reserve team. This team was comprised of healthcare heroes from a variety of clinical and non-clinical backgrounds who were temporarily reassigned to other facilities that needed extra assistance.
Meet Rebecca Reinold, a practice registered nurse at Family Medicine of Lindenhurst, Long Island, who was redeployed as a nurse practicing bedside patient care for six weeks at Plainview Hospital during the COVID-19 pandemic. This was a change from her day-to-day activities as a practice nurse but a role she embraced. “I felt an obligation to help as many people as I could—staff and patients alike,” says Rebecca.
Rebecca’s career journey before COVID-19
Rebecca started her career at Northwell as a practice office associate at General Pediatrics of Garden City in 2014. After graduating college as a registered nurse, she started working at Lenox Hill Hospital on the Orthopedic Unit. She then transferred to North Shore University Hospital to the Orthopedic Trauma Unit and has since left bedside nursing to be a practice nurse at one of our many physician practices. She is also currently pursuing her Master of Science in Nursing, Family Nurse Practitioner, at the Hofstra Northwell School of Nursing and Physician Assistant Studies with the assistance of Northwell’s tuition reimbursement program.
Career development during a critical time
During a pandemic, learning opportunities and professional skills development is not top of mind, yet Rebecca’s growth came in many ways at this critical time. Before going back to bedside care, Rebecca attended a refresher course that Northwell provided for those who wanted to brush up on their in-patient skills. Rebecca says, “My fellow nurses were very supportive if I had any questions regarding current protocols and practices.”
To ensure our team members and patients were safely cared for, all team members were fit tested and Northwell had ample personal protection equipment (PPE) available. Because of this, Rebecca stated that she never felt that her safety was compromised whenever she was at work. This created a safe work environment that allowed team members to feel comfortable.
During her reassignment, Rebecca held many duties but one stood out in particular. “One of the most significant roles that I held during my reassignment at Plainview Hospital was being able to help patients communicate with their families through video on an iPad,” says Rebecca. She felt a strong connection to her patients in this role because she also had a family member hospitalized at Northwell due to COVID. Rebecca was extremely grateful knowing her family member was provided the utmost care and that she was able to connect with them in the same way she connected her patients to their families to ensure they were not alone.
Once her reassignment at Plainview Hospital ended, Rebecca was temporarily reassigned to another internal medicine office in Woodbury, Long Island. Once again she had to adapt to a new location and policies due to the pandemic. She was grateful to be supported by leadership and her new team was very welcoming. Her role resumed as a practice registered nurse where she worked alongside the lead nurse and together they completed daily tasks such as medication refills, hospital follow-up calls, immunizations and assisting patients in the practice and by phone.
On the last day of her reassignment, Rebecca was surprised with balloons and treats for a sweet goodbye. “During my last day at Woodbury, the staff thanked me with a beautiful card and balloons.” This was an experience that Rebecca will never forget. “I would highly recommend joining the Reassignment Reserve team. It is a great way for healthcare providers to show how dynamic and versatile they are.”

Northwell is an organization that offers endless opportunities to its employees for pursing personal and professional development. Rebecca says, “I cannot say enough about how this organization has given me every opportunity to be the best version of myself.”
Get moving with an exceptional nursing career like Rebecca’s. Learn more about nursing at Northwell Health.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

The angel of environmental services
Written by: John Baez, Environmental Service Worker, Staten Island University Hospital
Environmental services is much more than keeping a clean environment. We are helping keep patients and their families remain comfortable.
I’ve faithfully worked for Staten Island University Hospital for 11 years, and travel three hours each way from my home in Yonkers on public transportation to help care for patients.
I’m not a clinical care provider, but my dedication to patient safety in the Environmental Services (EVS) Department is what I strive for. My coworkers and I are at the top of our field when it comes to bedside manner and being spirited patient professionals.
Unfortunately, our team is no stranger to a crisis. We saw the hospital through the evacuation ahead of Hurricane Irene, the aftermath from Superstorm Sandy the following year and even the Ebola crisis in 2014.
But COVID-19 was something entirely different and something we never faced before. It put the EVS team on the front line to help contain and eliminate the virus, which tested all of our abilities.
When the crisis was at its peak, I remember seeing one case after the other. People begging for their life, “I can’t breathe, I can’t breathe.” Before coronavirus, I would always try to befriend and comfort the patients. During the crisis, I showed them love when their loved ones couldn’t be at their bedside.
Then there was one day that would change me forever.
The faithful man
It was a regular day, and then one of patient care associates (PCAs) told me that this person is going to pass away. I knew the patient. I met her days earlier.
It was the end of my shift and I was ready to take my first bus home, but I said to myself “I can’t let this woman pass alone. I’m going to be there for her.”
I walked into the room and leaned over the patient and said, “It’s me, John. If you hear me, squeeze my finger. She did. I told her I want you to go with God. I want you to relax and once you see the light, I want you to go to it. I’m going to hold your hand until you go.”
The PCA cried alongside me.
I told the patient I would pray for her. On her third breath, she passed.
The doctor came in and checked her vitals, and confirmed what I already knew — she was gone.
I took the two busses and three trains home, replaying the day in my head. It’s always going to be with me and sad that she couldn’t have a loved one with her, but I couldn’t let her die alone.
I did what many health care heroes battling COVID-19 did: make the patients their second family and be their loved one.
During this crisis, my mother was begging me to quit because we’re dealing with something that’s new and scary. But we all have to be here. It’s our job. It’s what we signed up for.
John Baez works in the Environmental Services Department at Staten Island University Hospital.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

A humble hero of America’s COVID-19 response
Written by: Brian Donnelly
In one 29-hour period, a nurse practitioner assessed and treated some of the earliest COVID-19 patients in the US stuck aboard a cruise ship off the coast of California.
Bouncing back and forth in nautical step with the rough tide of the San Francisco coast, Bryan Lovejoy, DNP, 37, and his eight-person team passed under the Golden Gate Bridge; then the Bay Bridge in a small US Coast Guard patrol boat.
It was March 8, 2020.
“It was actually a nice little cruise when you get right down to it,” Mr. Lovejoy said, despite the sounds of seasickness surrounding him. “There were whales at one point, just kind of jumping around out there.”
Passing Alcatraz, the nurse practitioner at North Shore University Hospital (NSUH) — now farther than 3,000 miles from home — knew they were getting close to their destination — a 1,000-foot, 14-deck luxury cruise liner carrying 2,300 passengers and 1,100 crew members. The Grand Princess had been stuck 50 miles off the coast for days due to COVID-19 spreading rapidly among those onboard.
“I was kind of nervous about it. I saw the news,” he said. “The plan at the time was to try to keep this novel coronavirus out of the US as much as we could. Of course, we soon found out community spread was inevitable.”
The father of two and Smithtown, NY, resident is part of a 30-member disaster medical assistance team (DMAT). On behalf of the Department of Health and Human Services, DMAT responds to areas impacted by a health care crisis, like natural disasters, when local response capabilities are impaired.
In 2017 Mr. Lovejoy spent two weeks in both Houston and Puerto Rico in response to deadly hurricanes.
“You just don’t know what you’re going into entirely,” he said. “The situations are very dynamic.”
But, from March 8-9, an eight-person DMAT contingent faced a threat unlike any they had seen before.
“Our main objective was to identify how prevalent COVID-19 was on the ship before taking passengers off,” said Mr. Lovejoy, who joined DMAT in 2007. “Not many people had any experience with this virus yet, and definitely not on a cruise ship.”
Bryan Lovejoy treats a patient at North Shore University Hospital, where he is co-chair of the Collaborative Care Council for the advance care provider team.

Being prepared
Mr. Lovejoy’s coworkers at NSUH saw their first COVID-19 patient March 7, while he was heading out west to his next mission.
“Especially under the circumstances we are in during a crisis, it takes a leader like Mr. Lovejoy to put aside his personal priorities and become actively involved in a life-threatening mission like this,” said Susan Wirostek, nurse manager at NSUH.
There are two months each year during which a DMAT volunteer can be called into service, which is why Mr. Lovejoy keeps a bag packed with some basic necessities.
“You never really get used to it,” said Mr. Lovejoy’s wife, Dawn, 39. “Every situation is different. They’re all anxiety producing in their own way.”
The call for this latest mission came just before midnight on March 6. After spending a day with their kids, Julia, 9, and James, 5, he and Dawn were watching a movie — John Wick 2.
“Sometimes I have very limited notice,” he said, adding he still hasn’t seen the end of that movie. “I’m given my travel orders, I pack my bags and I’m out within a day going to wherever this is.”
Boarding the Grand Princess
Mr. Lovejoy was on a plane by 8 a.m. the next morning. Leaving his family, he said, is often the most difficult part of his work.
“This one definitely stood out as the worst,” Dawn added, “because as time progressed the virus got worse and worse here in New York. I was scared.”
With the Grand Princess in sight, the team of eight braved high swells and dangerous conditions to board a life raft sent to their US Coast Guard transport – the first of two “high consequence, zero margin transfers,” wrote Robert Kadlec, MD, assistant secretary for preparedness and response (ASPR), in a letter of commendation to Mr. Lovejoy.
“After safely boarding the Grand Princess, Mr. Lovejoy quickly demonstrated his clinical competencies and selfless focus on the mission as part of the HASTY rapid triage team, which executed near continuous operations for 29 hours, while wearing bio-containment equipment,” the high-ranking DHHS official wrote.
Jumping from the lifeboat onto the cruise ship ladder, Mr. Lovejoy’s team scaled the massive vessel, rung-by-rung.
“It’s big,” he admitted, quick to downplay the feet. “It didn’t take too long. I just remember thinking, ‘don’t look down and don’t let go.’”
Playing a crucial role
Starting near 7 p.m., Mr. Lovejoy worked through the night and into the next day, performing medical assessments and triage of more than 1,100 US citizens — breaking only for emergency rehydration. Mr. Kadlec wrote that their effort, “played a crucial role in the pre-positioning of critical medical assets, supporting personnel and operational planning by federal, state and local emergency responders.”
With his mission complete, the Grand Princess was allowed to dock and passengers to disembark from the ship. Those that showed symptoms of the virus had to be isolated and those that weren’t had to be quarantined — data now known thanks to Mr. Lovejoy and his team.
“And because of the nature of everything I ended up getting quarantined myself,” said Mr. Lovejoy, whose entire team spent 14 days at the University of Nebraska. “And fortunately we never ended up showing symptoms or getting sick.”
Both in quarantine and upon his return home and to work in late March, the lifelong Long Islander had a heightened fear, Dawn said, of contracting the novel virus.
“I have asthma, so I didn’t know how well I’d respond if I did get it,” Mr. Lovejoy added.
A quiet hero
When he left the Grand Princess March 9, there were 647 reported cases of COVID-19 in America, according to the Centers for Disease Control and Prevention (CDC). By the time he returned home March 23, there were more than 44,000 cases. That number nearly doubled when he returned to work a few days later.
Knowing this – and his particular risk — Mr. Lovejoy knew, still, where he needed to be. Like walking door-to-door on the Grand Princess, he floated from COVID unit-to-COVID unit at NSUH throughout the crisis, treating the explosion of patients showing up daily.
“When he went on the mission and when he goes to work every day, he knows how vulnerable he is,” Dawn said. “So, I consider him just a quiet hero, leading in his own way.”
Join the Northwell Health heroes keeping our patients and communities safe. Explore job opportunities.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

A team’s commitment to compassion strengthened through adversity
As COVID-19 restricted hospital visitations across the world, healthcare professionals at Northwell Health worked tirelessly to ensure patients knew they were never alone. With compassion as their motivation, our Northwell heroes on the frontlines quickly developed new ways to help keep patients connected with their families.
Nicole Ciccione, a nurse manager in the Pediatric Emergency Department at Cohen’s Children Medical Center, was moved by one of her colleague’s emails about the work being done at Long Island Jewish Medical Center. Inspired to act, Nicole and her team brainstormed different ways that they could help their fellow Northwell team members while improving the patient experience. “I reached out to my surrounding community to ask for toiletries to help our patients look, feel and smell fresh, and for different devices to assist with making virtual connections,” she says. The overwhelming response of donations was a refreshing reminder to her of the impact Northwell has made on the community it serves. With the donation of toiletries, iPads and other electronic devices, team members volunteered to not only connect patients with their families, but to spend time connecting with the patients themselves.
“There have been difficult times, sitting with a patient and their family on FaceTime, while the patient takes their last breath, to happier moments of connecting a patient with their family soon after extubation. For team members, it has been very humbling and rewarding to be able to help out not only patients, but also our LIJ colleagues. It’s connected our teams,” Nicole says, “I am proud to be the nurse manager of an extraordinary team that is willing and ready to help when called on.”
Debra Clifford, director of patient care services at Plainview Hospital, worked remotely during COVID where she found new ways to support her nursing staff and connect with patient families. She says, “The COVID-19 pandemic offered me the opportunity to get back at the bedside and help patients and their families in a different way than my current role. Working from home, I started to make calls to families to alleviate the frontline staff of the overwhelming calls that they were receiving from families. I gave daily updates, connected them with other disciplines in an attempt to stay connected to their loved one in light of a unique situation that echoed ‘no visitors.’” It was these moments on the phone delivering comfort to patients’ families that helped her feel connected even as she herself was away from the hospital. “My inspiration for working remotely soon came from the families that I had the pleasure of talking to each day.”
Marcy Hohorst, a family liaison at Plainview Hospital, also found new ways to deliver care as her Perioperative Unit was temporarily converted into an Intensive Care Unit. Having had experience working as a registered nurse in past mission trips, Marcy was uniquely prepared to deliver comfort and compassion as she helped patients connect to their families virtually. “It was and always will be my honor to have been able to connect families with their loved ones during their brightest moments or their darkest hours. This position was simultaneously meaningful, rewarding and heartbreaking. Someday, when COVID-19 is a distant memory, I will be proud to say, ‘I was the nurse with the iPad.’”
A commitment to health never stops and these individuals, as well as other team members across our organization, have demonstrated that nothing can stop them from providing the care patients and their families need and deserve.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Vicki is still helping patients and learning new skills after three decades in nursing at Northwell
During COVID-19 there were many changes at each hospital to accommodate the increasing needs for patients. Many healthcare workers also went above and beyond to treat patients by leveraging their skills in different ways.
Vicki Weyhreter, a Northwell nurse for 27 years, and her team members at Huntington Hospital began to see changes on their PACU floor. Typically, the PACU floor is where the patients go to recover temporarily from anesthesia after surgery. With the pandemic and temporary suspension of many surgeries, the PACU floor was transformed into a COVID critical care unit and Vicki and her team members were there to help in new ways.
Embracing new opportunities for patient care
As a seasoned healthcare professional, Vicki has impacted many lives during her career at Northwell and began her career as a Registered Nurse at Huntington Hospital in 1993. Throughout her career, she spent 13 years in the Intensive Care unit, eight years in the Recovery unit, and recently spent time in the Interventional Radiology unit. She has been fortunate to have many opportunities during her career to learn new skills and develop professionally. Vicki looked at her newest assignment during COVID as another opportunity to grow and help care for the patients in the community.
This assignment could not be accomplished alone—it required a team effort. Vicki and other PACU nurses were joined by anesthesia and trauma surgeons and physician assistants. Everyone worked collaboratively to optimize their skills, learn new tactics, and go above and beyond for their patients. Their strength came from the compassion they felt for their patients, which is what kept them going during this difficult time.
Vicki described seeing their patients giving a thumbs up or sitting in a chair as “the best feeling of our day.” When a patient is discharged from their unit, the team comes together to cheer and clap as they transition out of critical care.
Although the PACU unit will never be the same to most of the team members at Huntington Hospital, saving lives and embracing teamwork to provide the greatest care for the patient remains the same.
Vicki and her team members are truly Made for This, exemplifying the importance of their role in helping others fight the virus, and giving hope to their patients. Are you Made for a nursing career at Northwell? Learn more about nursing at Northwell Health.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Volunteering at a COVID-19 testing center in Manhattan was challenging yet rewarding
Written by: Chandra Bishun-Freeman, Senior Medical Assistant, Northwell Health Cardiology Upper East Side
My experience during the COVID-19 pandemic has been surreal yet terribly real. It has turned our world upside down. Life has changed — under different rules, protocols, even regulations. Like many others, this surreal experience started quickly for me.
For nearly every day of my married life, my husband would stop whatever he was doing to greet me at the door with a warm hello and a kiss when I came home. Our dog also sits patiently by the door, waiting to play. That was all gone in a matter of a few days.
Coming home after work, I run straight to the sink to wash my hands and change my clothes and shower. I greet my husband with an elbow bump. No more kissing or embracing. Our dog has to wait, sadly looking at me until I can give her attention. Since I was not sure if I was working with COVID patients at Northwell Health Cardiology, I followed the Centers for Disease Control and Prevention recommendations to practice social distancing at home. Bringing the virus home was a real fear, especially working in health care and traveling on subways and buses.
I’ve been at this cardiology practice for more than seven years, where I’ve focused on providing high quality patient care and support to my coworkers. I am a health care professional and a team player. I did not have a shred of doubt about my role. It is our calling, even if it means working outside normal routines. And in early March, I volunteered to work in one of Northwell’s hospitals that was most affected by COVID-19.
In about a week, I was redeployed to Northwell’s COVID-19 Testing Center on East 76th Street for four weeks in April. I was grateful to work on the front lines despite being fearful for my wellbeing and potentially bringing the virus home. Trying to fall back on my professional training, I ventured out in mask, gloves and worked six days each week, taking the nearly empty bus and train to and from work every day. As odd as this might sound, this was the work that I desperately wanted to do.
At the testing center, we performed nasal swab and blood testing for COVID-19 serology antibodies. The newly formed staff at the facility started training for nasal swabbing by practicing on one another. I was nervous knowing that someone would be putting a long and thin swab up my nose. I was only thinking about the pain and discomfort. Suddenly, I was a patient and a swabber-in-training. Having a swab inserted was the most uncomfortable feeling, but a necessary evil considering the circumstances. Doing it myself allowed me to calm patients and perform the test with precision and efficiency.
Despite the oversized white suit (PPE), I was still fearful of catching COVID-19. Most seven-hour days were spent in an isolation suit, along with a mask, gloves and face shield. What I remember most is how much I had to breathe my own bad breath. Coffee, onions, a bit of everything that went into my mouth would become something I inhaled for the rest of the day. As a swabber, my role was to stand in a room behind a plexiglass separation/protection to perform nasal swabbing. We treated every patient the same — assume they have COVID-19. Some patients came in with a fever. Others were very flush in the face. I remember one patient said to me “please don’t stand close to me. I am coughing and sick. I might be COVID positive.” Every patient, every moment was a heightened state of stress, focus and engagement.
Three days into working at the testing center, my husband told me my color was off. Most likely, I thought, because of wearing a mask, recirculating my own exhale for more than 12 hours. In another week, I had symptoms — runny nose, achy body and a cough.
Still, I enjoyed every moment working at the testing center, especially my colleagues. We made the best of the situation, offering light jokes to keep in the right mindset. During the four weeks working there, I met people from all over the health system. Leadership from Lenox Hill Hospital brought Bombas socks for each employee one day. There were free bagel breakfasts each Monday at another site across the city. Many of the patients I saw at the center were appreciative and thankful of the work I was doing, too, even those who indicated they felt ill and might be COVID positive. Although they were hidden behind their masks I could see how they genuinely felt by just looking at their eyes.
The long hours can wear on you. Waking up early was a part of it, considering I took an early train and crosstown bus to get there. I also volunteered to work 12-hour shifts on Saturdays. After the first Saturday, which followed a 40-hour week, every bone in my body ached, only remedied by a warm bath with Epsom Salt and an 8 p.m. bedtime.
By then, the mild symptoms I experienced a few days earlier worsened. My husband told me he had diarrhea and shortness of breath. Anxiety rose as I now was tested and eagerly anticipated the results while staying home. He and I pretended everything would be fine. And each day, each email or phone call, he would ask “is that the test result?” Luckily, I tested negative, a stress relief like no other. My husband and I kissed and hugged for the first time in what felt like weeks.
I also earned a recognition award from Northwell for working the front lines. Even with the fear of risking my own life, the sweat trickling down my body in the isolation suit, working the long hours, riding the early morning trains alone, without an ounce of doubt I would do this all over again. It was the right thing to do. But, in honesty, it will take the effort of thousands of front line workers who work each day to mitigate the impact of this pandemic. It’s a challenge worth fighting.
Chandra Bishun-Freeman is a senior medical assistant at Northwell Health Cardiology Upper East Side.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

How Northwell Health used medical research in the face of a global pandemic
Northwell Health implements innovation and technology to lead the industry. One of Northwell Health’s most valued resources is its home of medical research, The Feinstein Institutes for Medical Research. The Feinstein Institutes is comprised of more than 5,000 scientists and staff make groundbreaking discoveries in a number of areas such as, clinical trials, cancer, bioelectronic medicine and health outcomes. Researchers responsible for making key discoveries in autoimmune disease, sepsis, inflammation, and Parkinson’s disease, shifted their focus to help the fight against COVID-19.
As New York became the epicenter of the virus, the Feinstein Institutes went into action immediately. Within a month, Feinstein Institutes staff worked tirelessly to lay the groundwork to enroll more than 1,300 patients in seven clinical trials and programs. By collaborating with pharmaceutical leaders like Gilead, Sanofi and Regeneron, cutting-edge treatment was offered to Northwell Health patients hospitalized for COVID-19.
What’s worth noting here is not only the spirit of collaboration during a state of emergency, but the role medical research played in trying to find a reliable cure. As Dr. Kevin J. Tracey, CEO of the Feinstein Institutes notes, “Medical research will lead in our nation’s ability to reverse the fatal spread of viruses.” The Feinstein Institutes empowers its researchers and they are fully supported in their fields of practice where they are valued beyond measure. For Betsy Barnes, Feinstein Institutes investigator, the opportunities that have been available to her at Northwell have increased her industry knowledge and confidence in working around disease. So when it came to being called upon to help during a time of uncertainty around COVID-19, she was more than ready to begin research. When asked how it felt to know the impact of her work during a global pandemic, she explains, “It is a wonderful feeling to know I am able to apply my knowledge in a way that is beneficial to patients. We are doing everything we can to work quickly and collaboratively with hopes of producing knowledge that will cure COVID-19 and other health issues.”
The Feinstein Institutes partnered with the Mayo Clinic in joining a network that is working on novel, experimental therapy through the use of antibody testing for those who may have been identified with COVID-19, but are no longer asymptomatic. The incredible work wouldn’t be possible without the commitment its staff shares to delivering excellence. Excellence that inspires positive change for patients who trust Northwell every day. At the Feinstein Institutes’ Institute of Health Innovations & Outcomes Research, Professor Joseph Conigliaro, MD, gleams when speaking about his team. He says, “I am proud of the work my research team and I accomplished in such a short time for COVID-19 research – we are exhausted, but exhilarated and fulfilled in knowing conducting research is beneficial to patients in our health system, and to patients around the world.”
Working in the healthcare industry can be trying, especially when a global pandemic is added to the equation. However, with the leadership of Dr. Tracey and others who empower the imaginations of team members like Drs. Barnes and Conigliaro, the Feinstein Institutes will stand firm in their mission to produce knowledge to cure disease.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Lab Professionals play an essential role in the fight against COVID-19
Northwell Health Labs has been at the forefront of innovative care before and during COVID-19. Our labs quickly established itself as a leader in processing COVID-19 tests, being the first with manual tests, and later automated testing processes. As the fight against COVID-19 evolves, so does the work of our laboratory teams. Today their focus has shifted to include antibody testing, a test that allows patients to see if they previously had the novel coronavirus.
To perform these vital tests for our communities, our laboratory team members have been working in new ways. Former laboratory technologists have volunteered to return to the floor to help meet increased testing volume while our phlebotomists have been working outside the labs at COVID-19 testing sites. The teamwork displayed has been endless as they work together behind the scenes to keep our communities safe and our clinicians informed.
Recognizing the needs in this unprecedented time, many lab professionals continue to go above and beyond to deliver care. Merissa Ashrafalli, a lab technologist in Diagnostic Immunology/Serology at Northwell Health’s Core Lab, even returned early from her paid family leave bonding time to help support the fight against the virus. “I returned early to help on the front lines during this critical time because my team needed me. Our patients are our priority. Many think of a specimen as just a sample, but that is someone’s family member.”
And her work in Serology has never been more vital as her team works to get COVID-19 samples processed in a timely manner while dealing with new testing platforms and new assay material. “Without our staff in Serology, testing could not happen,” says Merissa. “As a team we are all working and learning together in this fight.”
Serology professionals aren’t the only ones essential to the Northwell Labs. Phlebotomists play the important role of collecting the samples – the first step in getting a diagnosis so patients can receive the care they need. As part of the initial battle, phlebotomists like Amber LaGuerre, volunteered to work at the New Rochelle COVID-19 testing site, the first in the country.
“Being a part of the New Rochelle drive-thru was a once-in-a-lifetime experience,” says Amber. “I jumped at the opportunity to volunteer because I knew it was my way to rise to the occasion and make a difference in this pandemic.” As the first testing site, the work of Amber and the other team members changed daily to ensure their testing would be as accurate as possible as the nation’s knowledge of the disease grew. It was their dedication, ability to adapt, and skills that helped make the site a success.
While Amber’s time at the testing site may have ended, she’s still working tirelessly to help patients get the care they need. As a phlebotomist with LabFly, Northwell’s mobile app that lets patients schedule blood draws at home, she’s bringing the testing process directly to our patients. “I know the work I’m doing is impactful no matter the setting I’m placed in, whether it be a hospital, nursing home, or a patient’s home,” says Amber. “Patients are more at ease being tested at home and I’m glad that we’re able to offer the convenience of LabFly to make the testing process just a little more comforting in a time of such uncertainty.”
Though work of our laboratory teams continues to evolve during the pandemic, one thing remains consistent: these healthcare heroes should be proud of the vital role they’re serving in defeating COVID-19.
“I am prouder than ever to work with Northwell Labs because I’ve seen lab personnel finally be recognized beyond the organization for the work we do,” says Merissa. “It is in these times that those who work behind the scenes get the thanks that is needed.”
“It’s very humbling to know as a phlebotomist my work is directly combating the fight against COVID-19,” agrees Amber. “The amount of gratitude I receive not only from patients, but people on the street that see me in scrubs throughout my shift, is a daily reminder of why I chose to be in healthcare.”
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Behind the Mask: Working as a Respiratory Therapist during the COVID-19 pandemic
Written by: Drew Devlin, RRT, LRCP, Director, Respiratory Care / Sleep Lab / Pulmonary Rehab, Southside Hospital
To say that the respiratory care team was instrumental throughout the COVID-19 pandemic would be an understatement. Although the respiratory care team has always been critical in patient care, it was in this pandemic battling a respiratory virus that the team had a moment to shine, and that is just what they did. Our respiratory therapists have touched every patient in one way or another by providing oxygen, running blood gasses, participating in intubations, managing ventilators, transporting patients to CT scans, and from emergency rooms to other critical care units. We have also been part of the process to meet the challenges of converting noninvasive ventilators into units that were now able to provide invasive applications. This team has truly been front and center playing a large part in caring for our patients during this period in an innovative way.
As the leader of the respiratory care team, I am truly proud of the work they did and how they stepped up to the plate during this difficult time of need. In order to deliver care during the outbreak, the work of the team evolved quickly and continued to change throughout the pandemic. Essentially, our normal process and daily responsibilities were completely revamped to adjust to the high volume of patients and the level of care we were providing to our patients. New policies, processes and protocols were developed rapidly and the respiratory care team was able to play a crucial role in the strategy and development of the new responsibilities. With respiratory therapists being so vital due to the nature of the illness, it gave them a great sense of purpose to be able to step in and provide their expertise. These healthcare heroes were truly able to make a major difference.

Respiratory care team members used posters to leave inspiring messages to each other throughout the pandemic.
Throughout stressful work conditions and long hours, team members found moments of hope and motivation by standing united together. I watched as they came to work every day with pain in their eyes and concern in their hearts for their patients, their colleagues, and their families, and yet they continuously provided the best care possible. There was camaraderie and collaboration throughout the whole process, and they really showed each other what it meant to not only be a team, but a family. To keep our spirits up, we would take time to share positive results of patients and track successful outcomes even after they left our care. There was also constant communication through emails, text messages, and postings on the walls throughout the department including pictures of the team hanging up as a constant reminder that we were all in this together. I also looked for articles on motivation to provide to the team and had the Chaplin come speak to the team in an effort to provide hope during this difficult time.
As a team, we also tried to talk about our experiences and share what we were going through to help each other out and know that we were not in this alone. We also brought in additional resources in the form of respiratory therapists from outside of the organization, to provide extra support and helping hands. This also enhanced motivation amongst the team because there was a realization that we were in a global battle, us versus the virus, and our best chance was to have all hands on deck and work together as a united team with respiratory therapists from near and far. It was also comforting and reassuring to see frequent visits from the senior leadership team to see how the team was doing, ask if there was anything we needed and how they could assist in any way.
The whole respiratory team exceeded expectations during this time, and I know this experience has made them stronger and even better than before. Each and every person on this team is my hero and we always consider ourselves a team and a family. Together, through this experience, they rose to the occasion and I am proud of the entire team for the work they have done and the care they have provided.

Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Personal connections make a difference
Written by: Elisa Vicari, LCSW, North Shore University Hospital
Staying in touch with families of COVID-19 patients have strengthened bonds and helped provide compassionate care against the odds.
As a social worker in the Intensive Care Unit at North Shore University Hospital, I’ve become immune to people passing away. Death is an unfortunate part of the job because we are treating the sickest patients.
COVID-19, though, was quite different for me and my colleagues.
During the patient surge in late March, we were caring for otherwise healthy 20- and 30-year-olds who were unaware of their surroundings and had no business being intubated. These are previously independent individuals who have been abruptly put on life support. This is the heartbreak the coronavirus leaves.
Adding to the complexities of this situation, visitation was restricted and patients in our unit were unable to speak to their families. This didn’t sit well, so I adapted my practice and refocused my efforts to find a solution. A quick Instagram post asking my friends and followers for one iPad donation turned into more than 20 and about $11,000 in community support — the true power of social media. Their assistance has allowed us to set up every unit within the hospital and other facilities in the area with iPads, which have been critical to helping us connect with families.
Not everyone is comfortable going into patient rooms. It’s a personal choice that must be made, one that I did not struggle with. A social worker’s role is to connect and assist, and the iPads have opened new roads to make important video calls where we could show not just a patient’s condition, but the entire room and care team.
In the ICU, patients are mostly intubated. Finding close connections has been challenging. Instead, we have grown closer to families, FaceTiming with them every other day for status updates, learning nicknames, favorite songs and of their pets who await them at home. They’ve sent pictures so we can build collages and fill their rooms with love. I feel like I’ve become a part of these families just by holding the screen for them.
In some end-of-life circumstances, visitors have been allowed to see their loved ones in their final moments. We’ve been there to help them with personal protective equipment (PPE), addressing their fears and coping with their situation. Some are able to hold their family member’s hand for the first time in weeks. We are also assisting with funeral arrangements, which are very different than usual with increased wait times. It’s overwhelming, physically taxing and mentally exhausting. But it’s worth it. I couldn’t imagine being on the other side, watching the terrible images on the news of beds being piled up and not knowing if my loved one is OK. Showing families that our patients are in private rooms and we are helping them has given them tremendous comfort.
When patients fail, I feel it more than I used to because I’ve grown closer to them and their families. Our conversations aren’t just based on medical concerns, rather vulnerable situations that I’ve now been welcomed into.
It’s bittersweet. When things go well, they go well. But when they don’t, it’s devastating. At the heart of it, we deliver personalized, patient-centered and compassionate care, pandemic or no pandemic. COVID-19 may have tested our mettle and capabilities, but we have survived thanks in part to the camaraderie between us and families. We have all met this challenge with innovation, compassion and integrity. I really admire the people I work with who have stepped up. Teamwork is everything, knowing we will get through this together.
Elisa Vicari, LCSW, is a social worker in the Intensive Care Unit at North Shore University Hospital.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Beyond the PPE: Two nurses help patients and staff connect during COVID
 Lulette Infante and Antonella Farrell, registered nurses at Northwell Health and lifelong friends, came together during the COVID pandemic to identify a solution for our clinical team members so they could maintain that personal connection during patient care. These two incredible nurses wanted to ensure that our patients would still be able to see the identities of our healthcare heroes, whose faces were covered by their personal protection equipment (PPE), so they created photo badges for our clinical staff to wear over their PPE.
Lulette Infante and Antonella Farrell, registered nurses at Northwell Health and lifelong friends, came together during the COVID pandemic to identify a solution for our clinical team members so they could maintain that personal connection during patient care. These two incredible nurses wanted to ensure that our patients would still be able to see the identities of our healthcare heroes, whose faces were covered by their personal protection equipment (PPE), so they created photo badges for our clinical staff to wear over their PPE.
The idea was prompted after reading a New York Times article featuring Cohen Children’s Medical Center’s Senior Vice President Dr. Schlein who acknowledged his gratitude to the frontline workers who saved his life from COVID, but he had no idea who they were because of their PPE. Thus, Project Unseen Heroes was formed so patients would be able to see the smiling, caring faces of our frontline workers.
A career journey that surpasses two decades
Both Lulette Infante, MSN, RN, CPON, and Antonella Farrell, BSN, RN, began their careers more than two decades ago as a student nurse intern from Adelphi University at CCMC in 1996. They advanced their careers at Northwell throughout their journey, holding a variety of roles and responsibilities along the way. Today, Lulette is an ambulatory nurse specialist and ambulatory administrator at Northwell where she focuses on quality and optimization for pediatric practices, and Antonella Farrellis is a pediatric Hematology/Oncology, pediatric sickle cell nurse coordinator at CCMC.
One small idea leads to big results
Lulette and Antonella first introduced the large photo badges at CCMC and Long Island Jewish Medical Center, receiving numerous positive responses from leadership, staff and patients. Lulette notes patients even commented, “so that’s what you look like!” Eventually they were able to guide other hospitals, including Northern Westchester, Lenox Hill, Huntington Hospital and even external hospitals such as Elmhurst Hospital, to develop photo badges for their team members.
“The staff is reporting back that they felt it is truly helping their patients now that they can see the smile behind the mask,” Antonella says. The staff has been sending Lulette and Antonella pictures of themselves in the PPE with their badges. Having the large picture badges enabled our frontline workers to maintain that personal connection while caring for their patients while being fully secured under their PPE at the same time.
“We could not even start without the incredible support we have received from our leadership and their commitment to continually enhance patient experience and promote compassionate care,” Lulette says.
Project Unseen Heroes was a success due to Lulette and Antonella’s teamwork. Patients feel more comfortable in the hospital seeing the badges on the nurses and doctors, knowing who is taking care of them.
Lulette and Antonella are true examples of Northwell Heroes. Are you ready to become a Northwell Hero? Join our team.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

How a new team delivers hope to COVID-19 patients at Northwell Health
Northwell Health has taken action to find ways that help deliver exceptional care to its patients affected by COVID-19. As many healthcare organizations search for ways to improve patient outcomes during this difficult time, Northwell has trained and equipped its teams to do that and more. One example of this is the formation of its Prone Teams.
Proning is a technique used to help patients breathe easier by changing their body position. As most patients rest on their backs while in the care of nursing staff, the Prone Team carefully places COVID-19 patients on their stomachs, allowing more air into the body and increasing oxygen levels into the lungs. As this technique is used in the operating room on a daily basis for certain surgical procedures, our Perioperative teams were chosen to help spearhead Prone Teams across the organization.
Comprised of perioperative RNs, surgical technologists, perioperative assistants, and physical therapists, our Prone Teams worked to safely turn and position patients into both the prone and supine positions and trained other team members on proper positioning. Implementing this new team during the COVID-19 crisis has proven how Northwell can meet even the biggest challenges with innovative thinking and utilize all team members’ skills to provide care.
Meet some of the team members from the Prone Team making a difference every day.
At Long Island Jewish Medical Center (LIJMC), the Prone Team features Christina Raccasi, an RN who joined Northwell as a graduate in 2018 and is currently a perioperative registered nurse. While new experiences always have initial challenges, Christina quickly overcame it due to the support and environment she works in. She states, “Caring for patients in a way that was outside of my comfort zone and training was a scary thought at first, but since many of the Prone Team members are from the operating room, we felt confident in our established teamwork as we work together so regularly.” Beyond just positioning, the Prone Team members deliver care in other ways outside of their usual scope in the OR, helping to protect patients with padding for bony prominences, lip moisturizer, and skin barrier cream.
Joined with Christina in the fight against COVID-19 is Dolores Reisert, Senior Administrative Director II of Perioperative Services, who helped form LIJMC’s Prone Team and shares the same sentiment. She states, “The teamwork among the perioperative and the ICU units is so inspiring and I am so proud of how this team was developed and trained so quickly. The Prone Team has been an asset in this important endeavor in trying to help our patients fight this terrible virus to aid them in the road for recovery.” Dolores joined LIJMC in 2015 with over 32 years of Perioperative experience, and even still, she is able to find more ways to advance her career and develop as a leader within her practice at Northwell. Today, she presently oversees six areas at LIJMC, the Operating Room, ASU, PACU, Endoscopy, Surgical Annex, and Central Sterile and has proven to be an incredible asset to the teams under her leadership.
Over at Huntington Hospital, OR Supervisor Jose Gonzalez’s leadership has proven itself to be equally as valuable to the Prone Team he oversees. While Jose’s usual day-to-day means ensuring the operating room runs smoothly, he stepped up to help lead Huntington’s Prone Team and trained additional team members to support the team and ensure it was running Monday through Sunday. His know-how made him a perfect leader for the team, and much like Dolores and Christina, the experience he brings to the room is what gives Northwell so much confidence in its ability to come out on top of this pandemic. “It’s a surreal feeling walking into these units and being thanked by the ICU team members who work tirelessly around the clock with critical COVID positive patients,” he says. He adds, “My team and I have been honored to be able to help our patients. Even though our patients are vented and may never get to know who we are, they have become our family.”
Each of these members play a role that, at the top of the year, they had no idea they’d be playing. Yet, because of their commitment to care, they have adapted and discovered new skills within their fields that will help heal our communities and bring new hope to the patients that entrust Northwell Health with their lives.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Delivering moments of peace on the front line with Tranquility Tents
As the rest of the nation stayed home to help flatten the curve of the COVID-19 pandemic, our healthcare heroes at Northwell Health continued to come in each day, fighting against the outbreak on the front lines of our hospitals. Their unwavering dedication and commitment to keeping our communities healthy had them delivering compassionate care, no matter the circumstances.
Seeing firsthand the tireless work of our team members, Northwell leadership immediately understood the importance of reflecting that same compassion back to our team members to meet their mental, physical and emotional needs. Working in health care, so much of your day can be devoted to giving to others and forgetting to take time for yourself. Our Employee Engagement team partnered with Human Resources, Wellness, Chaplaincy and Employee Assistance Program (EAP) teams across our health system and created Tranquility Tents at all of our hospitals to give team members a place to press pause.
These Tranquility Tents are designated spaces for our team members to find moments of peace and reflection, to recharge as they continue to push through these days to care for patients who need it the most. Beyond offering respite, these centers provide access and information for all the resources Northwell has to support them through this unprecedented time. Whether it’s a tired nurse looking for a quick recipe to make dinner after a long shift or a team member in need of 1:1 counseling with a behavioral health representative after a loss of a patient, Northwell’s Tranquility Tents have what they need.
EAP members are on site to help team members talk through what emotional support they might need along with providing printouts of the diverse resources offered. Wellness posters provide new tips each week including meditation guides, recipes and stretching suggestions to ensure our team members are taking care of themselves physically as well as emotionally. The Chaplaincy team performed blessing of the hands, hosted prayer circles, and created prayers and messages to deliver words of encouragement and to connect with team members spiritually.
“The Tranquility Tent started as an idea and a vision from our corporate HR partners and has truly taken on a life of its own in terms of providing emotional, mental, physical and spiritual support for our healthcare heroes,” says Lisa Khavkin, VP of Human Resources at Huntington Hospital. “They have become a place our team can rely on to find a shoulder to cry on, a place to pray, to stretch, listen to music, or paint a stone to memorialize their feelings. While the journey is still ahead of us all, the tranquility tent has become a place of solace and healing.”
Along with support resources, our Tranquility Tents also offer opportunities for team members to take self-care moments. From hiring a barber to give haircuts to arranging for live music to be played, our Tranquility Tents are becoming safe havens for team members to feel good together.
Other activities at the tents may include:
- Gratitude Rock Gardens: a therapeutic exercise for team members to reflect on what they’re thankful for during this time, memorializing their thoughts and gratitude while painting rocks to add to the site garden.
- Nametag Making Stations: where team members can design their own nametags to help bring a human element back to their personal protective equipment (PPE).
- Message of Hope Boards: a reflective exercise for team members to add inspirational messages while reading the heartfelt sentiments other team members have left behind.
- Color by Number Art Installations: that are allowing our Northwell team to ‘leave their mark’ by coloring in this interactive art piece. This small moment of art therapy will also transition into a lasting legacy of the impact they’ve had as the art is displayed at each site upon completion.
As we move forward as an organization from fighting against COVID-19 to recovery, these spaces will transform to continue to provide the resources our team needs. “Tranquility spaces will become permanent places within our facilities to enhance the recovery and resilience of our team members. We must continue to adapt our offerings to meet the needs of our team members” says David Gill, AVP of the HR Employee Experience team. As part of this commitment to support, a well-being survey was sent to all our team members to gain insight on what they need not just today, but in the future. This feedback is being utilized by a well-being work group that will continue to evolve the resources available to ensure our organization feels engaged and together.
Though our team members are facing an unprecedented battle on the front lines, we know that we can heal and move forward to a brighter future Truly Together.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Emergency room nurse helps patients recovering from COVID-19 feel right at home
When you think of excellent patient care, endless opportunities, and extraordinary teamwork, Northwell comes to mind. Ashley Sells, a registered nurse at Lenox Hill Hospital in the Emergency Room, exemplifies all of these qualities. She continually practices outstanding patient care and teamwork and especially during the critical times of COVID-19. It is during this time where Ashley went above and beyond for our recovering patients to help them feel at home by starting a “Pick-Me-Up-Pillow” fundraiser.
Ashley’s career journey
Ashley started her nursing career with Northwell eight years ago at Long Island Jewish Medical Center (LIJMC) as a medical surgical nurse, where she served for one year before transferring into the Emergency Room fellowship. Ashley spent two years at LIJMC there before transferring to Lenox Hill. “It was always a dream of mine to live in New York City and work in an ER and Lenox Hill was my ultimate goal,” she says.
Throughout her years at Northwell, Ashley has made a positive impact on leaders and team members as her career has developed. “I am proud to work for an organization that promotes self-growth. Personal input and ideas are always welcome, and leadership continues to assist on any way that they can,” she says. Ashley’s favorite thing about working in emergency medicine is that there always is the ‘unknown’ factor and an element of surprise. She states that, “Every day is a new day, a new learning opportunity. As a nurse, I am challenged each day that I step into work.”
Putting patients first always
During COIVD-19, Ashley took the initiative to raise money selling pillows to help patients feel as comfortable as possible while on the road to recovery. She was inspired by an unfortunate situation when her colleague was diagnosed with COVID-19 and was then admitted into the hospital. She wanted her colleague to feel as much like home as possible while recovering, even down to the pillow she was using. That prompted Ashley to bring her two of her own pillows.
“A simple pillow made her day!” Ashley says. After her colleague was discharged, she donated the two pillows to another patient who was in need. “After recognizing that a pillow could put a smile on a patient’s face, I developed the “Pick-Me-Up-Pillow” fundraiser in hopes that every patient could have the same opportunity to have a comfortable pillow while fighting COVID-19,” she says.
“We often say that the little things make the biggest difference,” Ashley says. Ashley’s fundraiser has raised $5,000, enabling her to purchase 1,200+ pillows that were delivered to Lenox Hill Hospital patients. “This initiative has made me feel proud. This is something that I was personally able to accomplish because of the generosity of others,” Ashley says.
Ashley’s work embodies the Truly Compassionate care that Northwell values. “The outpouring of support our community has shown during this time has been so valued by the Northwell staff. The endless food donations, the letters of encouragement, the 7 PM clap has truly helped to motivate and inspire our team,” says Ashley.
Ashley is a healthcare hero, showcasing her willingness to go above and beyond for our patients. Are you Made for nursing careers? Join our team of heroes.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Braving uncertainty during uncertain times
Written by: Cassidy Toben, Assistant Nurse Manager, Emergency Department, Lenox Hill Hospital
Northwell Health is proud to spotlight our front line health care workers. See how Northwell clinicians – doctors and nurses – are responding and working on the front lines of the COVID-19 pandemic. Read their stories here.
Cassidy Toben, RN, finds a new niche as COVID-19 forces health care workers to shift roles
As an assistant nurse manager, I’m lucky to have the opportunity to inspire and motivate our nurses and staff, really coach them through their nursing journey. And during the COVID-19 crisis, my role has shifted, transitioning into even more administrative responsibilities.
I’m not always in the rooms with COVID patients, and there’s a sense of guilt that comes with that. Togetherness and camaraderie are built within nurses. It’s our calling — caring for another as if we are the patients we are restoring to health. Leading my team is also a calling, one that I’ve relished during this situation.
Since COVID-19 reached our doors at Lenox Hill Hospital, we’ve bundled care, limiting the number of people and trips in and out of patient rooms. What you might do in a few trips, you do all at once now.
On tough days, and there have been many, one of my nurses will need me to serve as a sounding board to vent about harrowing experiences, or to cry with them about a lost patient. Being this support system is critical to their well-being. We all share the burden and have a stake in this.
I went into nursing to save lives and to help people. But, you realize quickly that you can’t save everybody. That’s really humbling.
The scariest day during this experience came at the end of March. New York was just hitting its peak and COVID-19 patients arrived at alarming rates. One patient was talking to us and seemed pretty stable. About an hour later he coded. Everybody ran to his bedside. Then about 10 minutes after that, a patient on the other side of the emergency department coded — everyone ran to that bedside.
Then a third patient needed resuscitation.
 I took a step back and, while watching every one race to the bedside, thought to myself, “Wow, the teamwork here is really inspirational.” The compassion that they showed to the patients, to each other, it eased my fears that day. We have each other’s backs and we support each other. We take care of our patients and we go home. Most of us go home alone. We don’t get to hug our parents. We don’t get to see our families. So, we’re really in this together.
I took a step back and, while watching every one race to the bedside, thought to myself, “Wow, the teamwork here is really inspirational.” The compassion that they showed to the patients, to each other, it eased my fears that day. We have each other’s backs and we support each other. We take care of our patients and we go home. Most of us go home alone. We don’t get to hug our parents. We don’t get to see our families. So, we’re really in this together.
But worry does come over the staff. Patients begin to remind you of your family — many times you’re acting as their family, with visitation suspended in hospitals. And then you worry about your own family, and then yourself.
(Deep breath)
My first symptoms started on March 26, a curious cough that would lead into fatigue and shortness of breath. My husband and I decided it would be safer to stay together than risk exposing anybody else in my family. Still, the thought of getting him sick caused so much anxiety that I started having nightmares. I dreamt that I got him sick and he was dying, because that’s what we were seeing each day. And any health care worker can tell you that they have that exact same fear. It’s not about me. I can handle me. But I don’t want to hurt the people I love.
After two weeks of being ill, I returned to work. I still struggle to sleep, but now it’s our patients that I worry about. It’s also really rewarding to see that our staff has risen above a lot of the challenges, remaining positive at every corner. So, even on days when I’m operating on little sleep, I come into work feeling like we can succeed. We are together and we’re going to get through it.
Luckily, the situation has improved — the volume in the emergency department has slowed. People are staying home, and we’re now on the right part of the curve. Devastation has turned into hope. We’ve lost a tremendous amount, people we know, grandparents, friends. So, we must remember those who are lost and work through each day with positivity.
In a time where it’s hard not to think about yourself and your family and worry about getting sick, people are still thinking about each other here. That is just absolutely incredible. It makes it all worthwhile, providing purpose and an unrelenting desire to help another.
That’s what nursing is truly about.
Cassidy Toben, RN, is an assistant nurse manager in Lenox Hill Hospital’s emergency department.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Written by: Colleen Conaty BSN, RN-BC, Float Team, North Shore University Hospital
Behind the Mask: Working as a Float RN during the COVID-19 pandemic
Being clinical professionals, we were excited and honored to be a part of history by saving lives – but we could not have anticipated what the next weeks would bring. Though it was unlike anything we could have imagined, my team managed our small unit like champions. As the first designated unit, we were also the first to use personal protective equipment (PPE). We then used our experience to start the education process to teach others how to don and doff PPE properly. From respiratory therapists and environmental service workers to doctors and advanced clinical providers the float team was there to educate them all. We wanted to make sure each member of our North Shore University Hospital (NSUH) team would be able to fight this battle safely.
As the need for more COVID units arose, we opened our unit happily to the ICU nurses who expanded their services to care for patients. We showed them where our supplies were kept and oriented them to our unit so they could take care of the sickest patients. The float team’s challenge was then opening two brand-new units and our nurses, PCAs and CSAs, proudly came in on days off to help support our patients. Every time a manager would ask for more staff many volunteers would offer each time – all to make sure our team members weren’t going to be overwhelmed.
We are still fighting, but the most amazing thing I’ve noticed over the past weeks isn’t just the amount of lives we’ve saved, but that everyone is still smiling. My team carries on with the same smiles and laughs they’ve always had, sending each other heartfelt messages throughout the day. Come to one of our units at any time and I guarantee you’ll hear uplifting music playing from our nursing stations. You’ll find a busy nurse still making time to go room to room with an iPad, helping our patients to FaceTime their family. A few happy tears are shed when we learn a patient has been discharged or when we hear “Here Comes the Sun” play overhead, and celebrating that a patient gets to live because they won the battle – that we won the battle together.
I have never seen strength like this in my lifetime. Though these times are dark, this team has brought light into this world and shown me what it means to truly be a hero. Working aside these people has been the privilege and the honor of a lifetime. Float team, you are saving lives every single day and going through one of the hardest times, arguably of our lifetime, and you’re facing it with positivity. I am so proud of you all and so proud to call you my float family.
![]() Are you Made for an exceptional nursing career like Colleen’s? Learn more about nursing at Northwell Health.
Are you Made for an exceptional nursing career like Colleen’s? Learn more about nursing at Northwell Health.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Joining the fight: Meet Alison Laxer, MD
Northwell Health is proud to spotlight our front line health care workers. See how Northwell clinicians – doctors and nurses – are responding and working on the front lines of the COVID-19 pandemic. Read their stories here.
After graduating early from the Zucker School of Medicine, Alison Laxer, MD, is entering the effort to care for COVID-19 patients.
March 25 is a day I will never forget. Not because I celebrated my birthday with my family, but because I learned something that would change my life forever.
Late that Wednesday evening, I received a message about a Zoom virtual meeting with Lawrence Smith, MD, MACP, dean of the Donald and Barbara Zucker School of Medicine, where I was well into my fourth year. We usually don’t have meetings with the dean like this, but under the current circumstances, anything was possible. Dr. Smith told us we are graduating early and have the option to join the fight against the coronavirus.
My parents, who are both physicians, were nervous. And rightfully so. Who would want their child to voluntarily be exposed to COVID-19? But they understood and would’ve taken the opportunity to do the right thing if they were in my situation. We are physicians after all. This is what we signed up for.
My boyfriend, Alexander Smith, MD, who is also in my class, had similar feelings about the decision — he said we can be a part of history. We both decided independently, and it was never a question of if to do it, but when do we start?
The truth is, I will start in a few days. I finished virtual training earlier this week. Fear. Excitement. Concern. There’s a wide range of emotions flowing. We know we won’t see our families. We know we should avoid highly populated places like grocery stores. But we also know that we can help make a difference for so many struggling with the pandemic.
They say your fourth year of medical school is supposed to be a glorious time. Alex and I had plans to go to Europe, then the Caribbean, then to my cousin’s home in Chicago. It was supposed to be a time to really relax and rest before starting my residency at Cohen Children’s Medical Center. It’s strange that I will be spending this time at a hospital rather than a beach. But if this is what is needed, I’m going.
To say I’m scared would be an understatement. This is something we have never done before and I think I’m more nervous about not being very helpful. I know Northwell has plenty of personal protective equipment. And I can see the camaraderie among staff who are celebrated and sharing their experiences in the media. I just want to play my part.
This virus has touched so many lives. I never thought being a doctor was a hazardous profession, not like a firefighter or policewoman. But we will be exposed and our mission has never been greater. Hopefully, this will encourage more people to go into medicine.
Alison Laxer, MD, is a recent graduate of the Donald and Barbara Zucker School of Medicine. After assisting in the fight against COVID-19, she will assume her pediatric residency.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016

Connecting with coronavirus patients, and their families
Northwell Health is proud to spotlight our front line health care workers. See how Northwell clinicians – doctors and nurses – are responding and working on the front lines of the COVID-19 pandemic. Read their stories here.
Nicole Fishman, RN, isn’t just caring for COVID-19 patients at Huntington Hospital, she’s helping them communicate with their families too. Hear her story.
During the COVID-19 crisis, there’s been an even greater focus on caring for our patients as whole people in light of very limited visitation policies. They sometimes get scared having minimal contact with their friends and families. But my staff and I have been proactively calling family members and giving them updates on their loved one throughout the day. We are also using iPads and tablets to Facetime and Skype with families, so they can share their love with our patients.
When we are communicating with families through tablets, I think about my own parents and how I would want them to be treated if they were in this situation.
It’s been amazing getting so much support from throughout our hospital. All of the people are are caring for are either suspected or confirmed COVID-19 patients. So everyone is isolated and requires a higher level of care. We are managing this by working as a team, staying strong and supporting each other in any way that we can. As expected, we’re taking everything day by day.
Wearing all of this additional gear can make it harder to breathe, which is why we need more frequent breaks. I try to take advantage of any time away, going outside for fresh air and to clear my head.
All of Huntington Hospital’s employees have been so appreciative of the meals that we’ve received from community donations. It’s been very helpful to not have to worry about cooking or preparing food. We can focus on what matters most — our patients.

One thing I’ve been surprised about is that younger patients — people in their 40s, 50s and 60s — are deteriorating faster than I would have anticipated. Some don’t have a past medical history of pre-existing conditions.
I’m fortunate to have a very supportive boyfriend who’s at home cooking and taking care of things while I’m out fighting COVID-19. Many of the other nurses on my unit have supportive significant others who have been writing encouraging letters and packing food for us.
When I leave work, I take several precautions in an attempt to protect my boyfriend from this dangerous virus. I change my shoes before I get into the car and shower immediately when I get home. I take all of my clothes off right by the door and throw them straight into the washing machine on a hot water setting. I feel safer being on my unit versus out in the community because we’re all wearing the proper protective gear and the unit is constantly being cleaned.
As advice from someone who has witnessed the devastation COVID-19 causes, please listen to what everyone’s saying. Stay home. Only then can people hopefully stay out of the hospital. If you don’t have to go out, please don’t.
Even though the world seems on hold right now, for health care workers it’s more like business as usual. Caring for our patients in all circumstances is what we’re made for.
Nicole Fishman, RN, is a nurse manager at Huntington Hospital.
Share this entry
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Subscribe to our blogs
Stay up to date with stories you want to know more about right to your email inbox.
Newsletter
Recent Posts
- Northwell is proud to announce the launch of The Management Accelerator and the Executive Leadership Program in partnership with McKinsey and Company
- Prioritizing Self-Care and Well-being at Northwell Health
- La’Dreamer Lark, Patient Access Service Representative and Community Captain
- Jennifer Tutone experiences nearly three decades of career growth as a clinician at Northwell
- Think Hospitality. Think Healthcare. Getting students ready with our Hospitality in Healthcare Internship at Northwell Health
Categories
- ACP
- Advanced Practice
- Advice Articles
- Appointment with…
- Benefits
- Cancer Care
- Clinical Care
- Clinical Laboratory
- COVID-19 Stories
- Culinary and Food Services
- Culture
- Diversity & Inclusion
- Emergency Medicine
- Employee Stories
- Events
- Featured Articles
- General
- HMP Internship
- Information Technology
- News
- Non-Clinical Professionals
- Northwell Community
- Northwell Ventures
- Nursing
- Nursing Education
- Nursing Support
- Patient and Customer Experience
- Perioperative Services
- Physician Assistant
- President's Awards
- Radiology
- Rehabilitation
- Research
- Spark
- Spotlight
- Students and Internships
- This is Healthcare
- Veteran
- Wellness
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Archives
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
Contact us
If you are an individual with a disability requesting an accommodation for the application process, please click the contact us link above to request assistance.
Learn more about our hiring experience.
Read answers to common questions about the application process.
© 2021 - Northwell Health
Click here to view the “EEO is the law” poster.
If you are an individual with a disability requesting an accommodation for the application process, please click the contact us link above to request assistance.
Learn more about our hiring experience.
Read answers to common questions about the application process.
© 2021 - Northwell Health
Click here to view the “EEO is the law” poster.
It is Northwell Health’s policy to provide equal employment opportunity and treat all applicants and employees equally regardless of their age, race, creed/religion, color, national origin, immigration status or citizenship status, sexual orientation, military or veteran status, sex/gender, gender identity, gender expression, disability, pregnancy, genetic information or genetic predisposition or carrier status, marital or familial status, partnership status, victim of domestic violence, sexual or other reproductive health decisions, or other characteristics protected by applicable law.
Northwell Health reserves the right to amend all terms of employment.







